1. What are cholinergic agonists and how do they function?
2. Neurotransmission at cholinergic neurons
3. Cholinoceptor stimulants & cholinesterase inhibitors
Drugs that affect the autonomic nervous system (ANS) are classified into two groups based on the type of neuron involved in their mechanism of action. Adrenergic drugs act on receptors stimulated by norepinephrine or epinephrine, whereas cholinergic drugs act on receptors activated by acetylcholine (ACh). Cholinergic and adrenergic drugs work by either stimulating or blocking ANS receptors. So cholinergic agonists can be defined as a class of drugs that affect the (ANS), particularly the parasympathetic system, by mimicking or modifying (ACh), which is why they are also known as (cholinomimetics) or (cholinomimetic drugs) (parasympathomimetic).
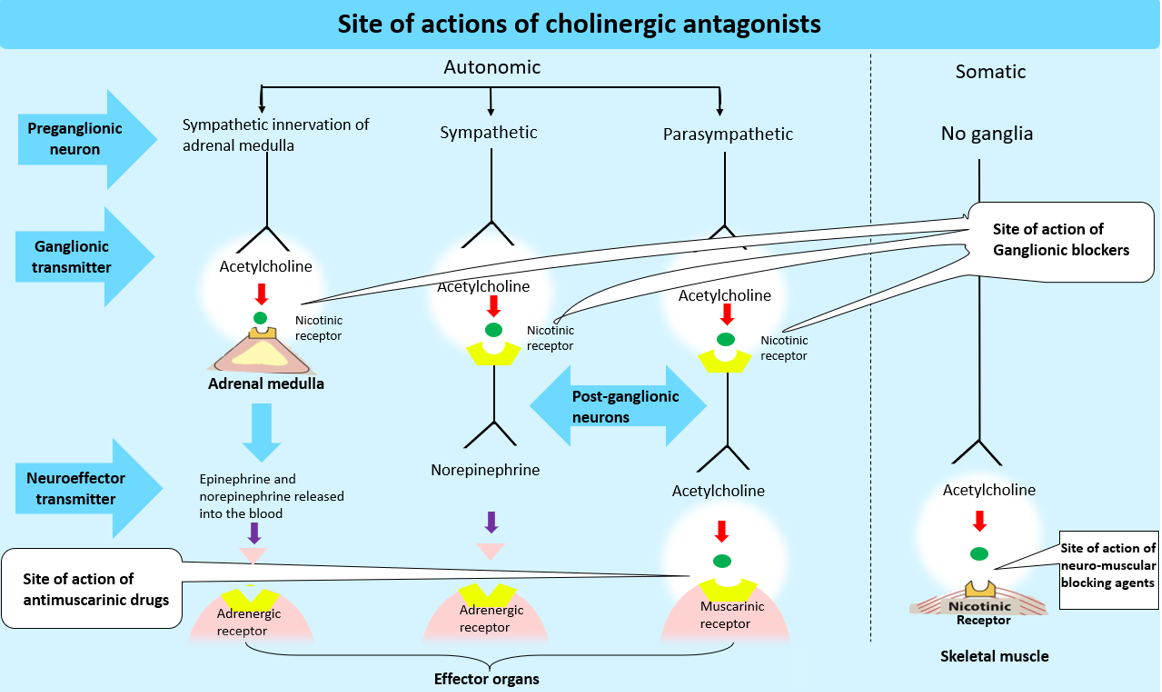
Acetylcholine (ACh) is the primary transmitter in all autonomic ganglia (parasympathetic and sympathetic) as well as at synapses between parasympathetic postganglionic neurons and their effector cells. It is the transmitter at the preganglionic fibers that terminate in the adrenal medulla, as well as the postganglionic sympathetic neurons in the thermoregulatory sweat glands. It is also the primary transmitter at the somatic (voluntary) skeletal muscle neuromuscular junction, and it plays a critical role in the central nervous system (CNS).
Six sequential steps are involved in neurotransmission in cholinergic neurons: 1) synthesis, 2) storage, 3) release, 4) binding of ACh to a receptor, 5) degradation of the neurotransmitter in the synaptic cleft (that is, the space between nerve endings and adjacent receptors located on nerves or effector organs), and 6) choline and acetate recycling These steps can serve as possible targets for pharmacologic therapy.
Acetylcholine is synthesized in the nerve terminal by the enzyme choline acetyltransferase (ChAT) from acetyl-CoA (produced in mitochondria), and choline is transported from the extracellular fluid into the cytoplasm of the cholinergic neuron by an energy-dependent carrier system that also cotransport sodium and can be inhibited by the drug (hemicholinium). [Note: Because choline has quaternary nitrogen and a permanent positive charge, it cannot diffuse through the membrane.] The rate-limiting step in ACh synthesis is choline uptake. Choline acetyltransferase catalyzes the reaction of choline with acetyl coenzyme A (CoA) in the cytosol to form ACh (an ester).
The vesicle-associated transporter, VAT, actively transports acetylcholine into its vesicles for storage. Another research drug may be able to inhibit this process (vesamicol). ACh is packaged and stored into presynaptic vesicles by an active transport process coupled with proton efflux that transports ACh into presynaptic vesicles. Aside from ACh, the mature vesicle also contains adenosine triphosphate and proteoglycan. Autonomic neurotransmission is the norm rather than the exception. This means that most synaptic vesicles contain both the primary neurotransmitter (in this case, ACh) and a cotransmitter that either increases or decreases the effect of the primary neurotransmitter.
The release of transmitter stores from nerve-ending vesicles necessitates the entry of calcium through calcium channels. When an action potential propagated by voltage-sensitive sodium channels reaches a nerve ending, voltage-sensitive calcium channels on the presynaptic membrane open, causing an increase in intracellular calcium concentration. Calcium increases the fusion of synaptic vesicles with the cell membrane and the release of their contents into the synaptic space. (Botulinum toxin) can prevent this release. The toxin in black widow spider venom, on the other hand, causes all of the ACh stored in synaptic vesicles to empty into the synaptic gap.
ACh released from synaptic vesicles diffuses across the synaptic space and binds to postsynaptic receptors on the target cell, and to presynaptic receptors on the neuron membrane that released the ACh's, or other targeted presynaptic receptors. The postsynaptic cholinergic receptors on the surface of effector organs are classified as muscarinic or nicotinic. Binding to a receptor causes a biological response within the cell, such as the initiation of a nerve impulse in a postganglionic fiber or the activation of specific enzymes in effector cells, which is mediated by second messenger molecules.
Because acetylcholinesterase (AChE) cleaves ACh to choline and acetate in the synaptic cleft, the signal at the postjunctional effector site is quickly terminated. Neither of which has a significant transmitter effect and thus the transmitter's action is terminated.
Because acetylcholinesterase is abundant in most cholinergic synapses, the half-life of acetylcholine molecules in the synapse is very short (a fraction of a second). Acetylcholinesterase is found in other tissues as well, such as red blood cells. (Other cholinesterases with a lower acetylcholine specificity, such as butyrylcholinesterase [pseudocholinesterase], are found in blood plasma, liver, glia, and many other tissues)
A sodium-coupled, high-affinity uptake system that transports the molecule back into the neuron can recapture choline. It is then acetylated into ACh, which is then stored until it is released by a subsequent action potential.
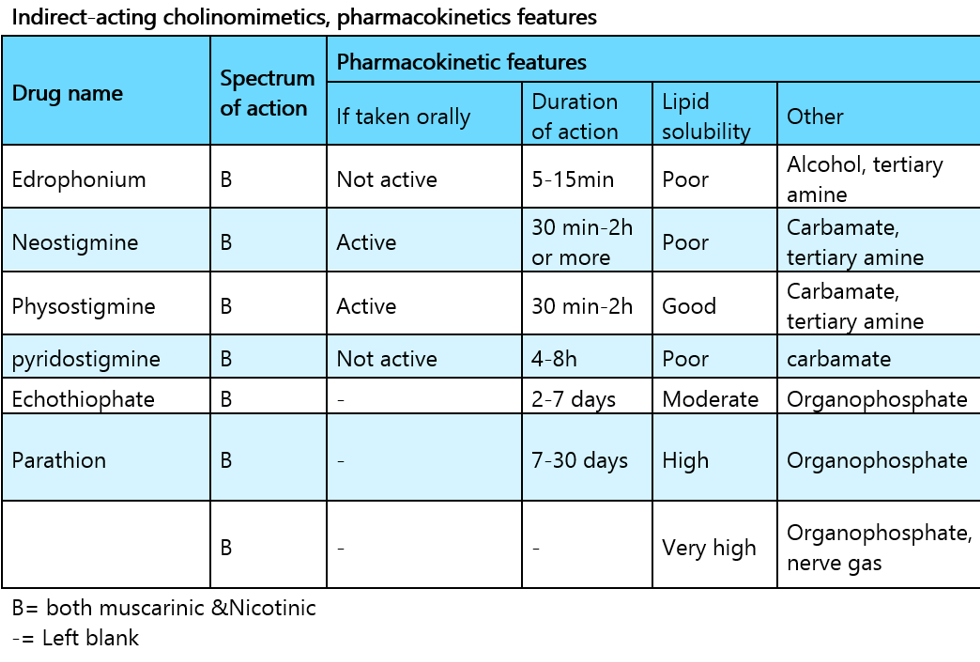
Acetylcholine-receptor stimulants and cholinesterase inhibitors are two types of acetylcholine-mimicking drugs (cholinomimetics). Cholinoceptor stimulants are classified pharmacologically based on their spectrum of action, which is determined by the type of muscarinic or nicotinic receptor that is activated. Cholinomimetics are also classified by their mechanism of action because Some cholinomimetics bind directly to (and activate) cholinoceptors, whereas others act indirectly by inhibiting the hydrolysis of endogenous acetylcholine. Acetylcholine can be thought of as the prototype because it acts directly on both muscarinic and nicotinic receptors. Neostigmine is a prototype for cholinesterase inhibitors that act indirectly.
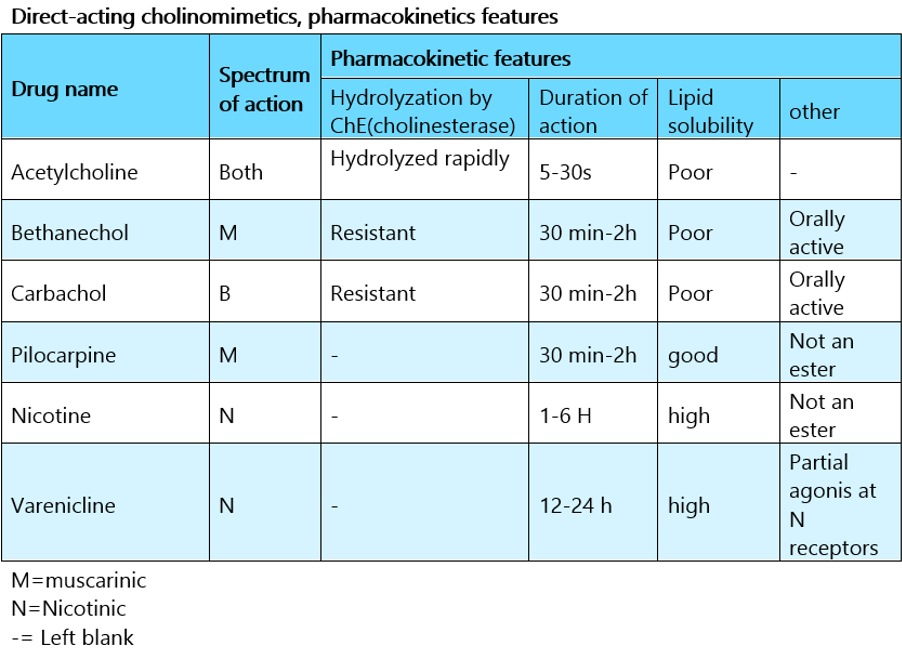
Are cholinergic agonists mimic the effects of ACh by binding to cholinoceptors directly (muscarinic or nicotinic). Direct-acting cholinomimetic drugs are classified into two groups based on their chemical structure:
Newer drugs are introduced regularly for specific applications. The members differ in their pharmacokinetics and their spectrum of action (the amount of muscarinic versus nicotinic stimulation). Both of these factors have an impact on their clinical application.
Because choline esters are hydrophilic, they are poorly absorbed and distributed in the central nervous system. Even though they are all hydrolyzed in the gastrointestinal tract (and thus less active when taken orally). All direct-acting cholinergic drugs have longer half-lives than Ach. They differ significantly in their susceptibility to cholinesterase hydrolysis.
Because (acetylcholine) is rapidly hydrolyzed, large amounts must be infused intravenously to achieve concentrations high enough to produce detectable effects. A large intravenous bolus injection has a brief effect, usually lasting 5–20 seconds, whereas intramuscular and subcutaneous injections have only local effects. (Methacholine) is more resistant to hydrolysis, and carbamic acid esters (carbachol and bethanechol) are even more resistant to cholinesterase hydrolysis and have correspondingly longer durations of action. The β-methyl group (methacholine, bethanechol) reduces these drugs' potency at nicotinic receptors.
Most administration sites absorb tertiary natural cholinomimetic alkaloids (pilocarpine, nicotine, lobeline). Nicotine, as a liquid, is lipid-soluble enough to be absorbed through the skin.
(Muscarine) is a quaternary amine that is less completely absorbed from the gastrointestinal tract than tertiary amines but is still toxic when consumed in certain mushrooms and even enters the brain.
(Lobeline) is a nicotine-like plant derivative. These amines are primarily excreted by the kidneys. Urine acidification hastens the clearance of tertiary amines.
Check out the cholinergic agonist drugs article to better understand the mechanism of action, therapeutic use, and side effects of each of those direct-acting cholinergic drugs.
1. Whalen, K., Finkel, R. and Panavelil, T.A. (2015). Pharmacology. Philadelphia: Wolters Kluwer.
2. Katzung, B.G. (2018). Basic & clinical pharmacology. 14th ed. New York I 11 Pozostałych: Mcgraw-Hill Education, Copyright.
3. Rosenfeld, G.C. and Loose, D.S. (2014). Pharmacology. Baltimore, Md: Lippincott Williams & Wilkins.
4. Trevor, A.J., Katzung, B.G. and Marieke Kruidering-Hall (2015). Pharmacology examination & board review. New York: Mcgraw-Hill.
Cholinergic agonists act similarly to Acetylcholine, either by directly interacting with cholinergic receptors or by increasing ACh availability at these sites.

The term "cholinergic antagonist" refers to agents that bind to cholinergic receptors (muscarinic or nicotinic) and block the effects of acetylcholine
The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)
Choose what we can use. Strictly necessary and security cookies are always on.