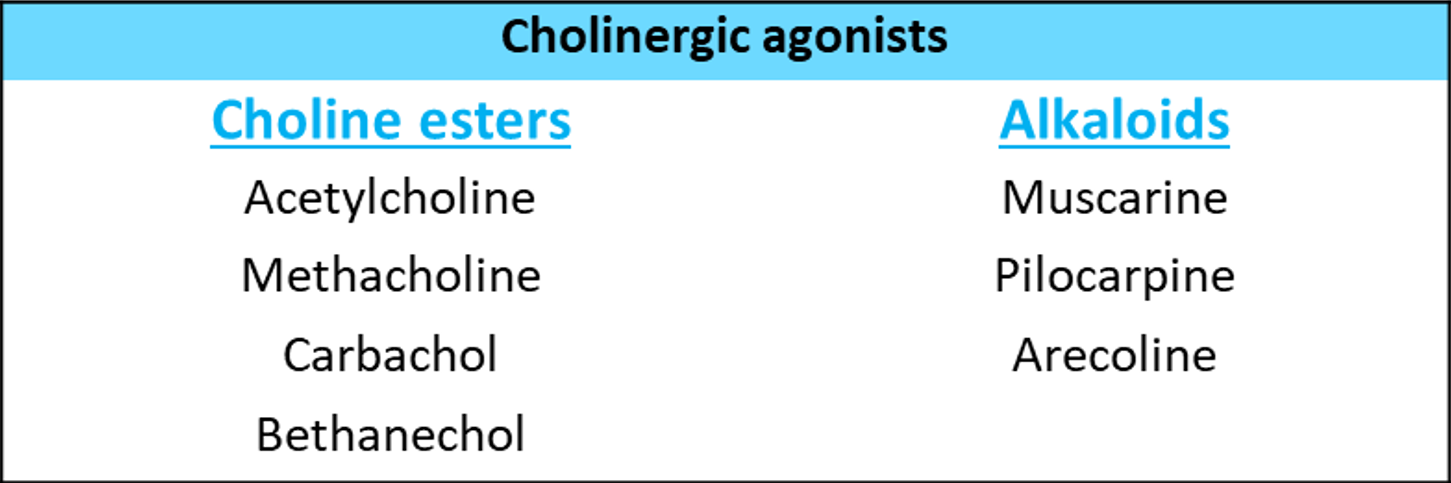
These are medications that act similarly to ACh, either by directly interacting with cholinergic receptors (cholinergic agonists) or by increasing ACh availability at these sites (anticholinesterases).
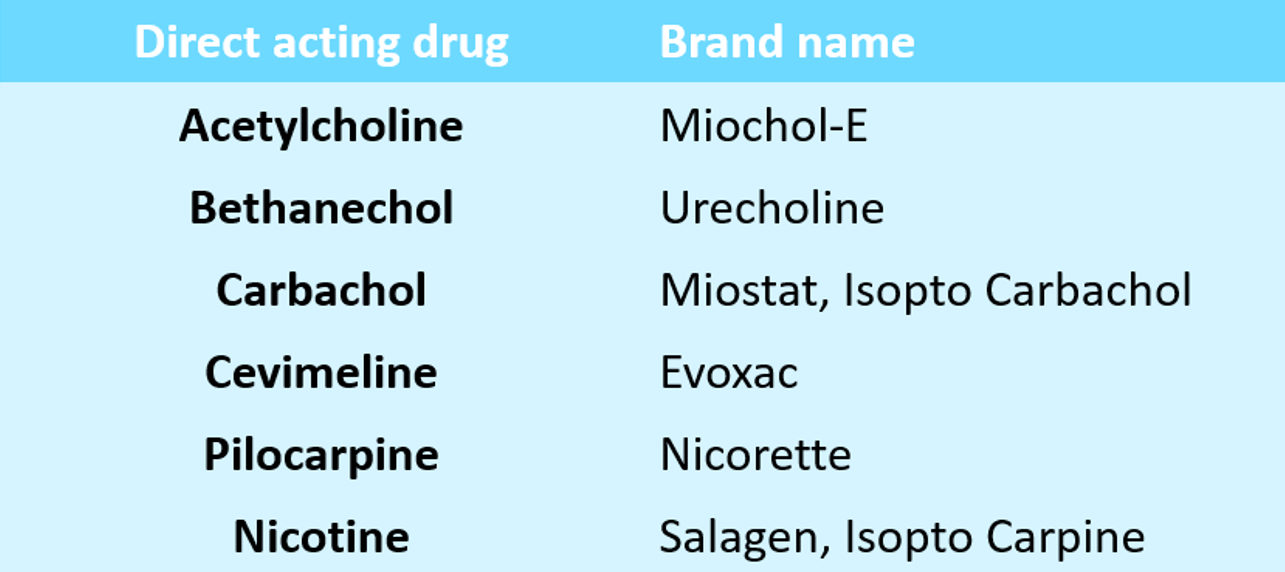
As we mentioned in What are the cholinergic agonists, and how do they work article. Direct-acting parasympathomimetic drugs act on (muscarinic or nicotinic) cholinoceptors to mimic many of the physiological effects of parasympathetic ANS stimulation. The most commonly used direct cholinergic agonists drugs.
Acetylcholine is a quaternary ammonium compound that is unable to pass through membranes. Although it is a neurotransmitter of the parasympathetic and somatic nerves, as well as the autonomic ganglia, it is not therapeutically important due to its diversity of actions and rapid inactivation by cholinesterases. ACh has both muscarinic and nicotinic activity, depending on the type of receptor through which it is mediated; therefore, ACh's peripheral actions are classified as muscarinic or nicotinic. The central actions, on the other hand, are not so easily classified and are described separately. Acetylcholine actions:
The effects of ACh on the heart are similar to those of vagal stimulation. ACh, for example, causes a brief decrease in cardiac rate (negative chronotropy) and stroke volume when injected intravenously due to a decrease in the rate of firing at the sinoatrial (SA) node. [Note: The release of ACh at the SA node regulates the heart during normal vagal activity.]
Although all blood vessels dilate, only a few (the skin of the face, neck, and salivary glands) receive cholinergic innervation. There is a drop in blood pressure and flushing, particularly in the blush area. ACh injection causes vasodilation and blood pressure reduction through an indirect mechanism of action. ACh activates M3 receptors found on endothelial cells lining blood vessel smooth muscles. Vasodilation is primarily mediated by the release of an endothelium-dependent relaxing factor (EDRF), arginine-derived nitric oxide. Nitric oxide then diffuses to vascular smooth muscle cells, where it stimulates the production of protein kinase G, resulting in hyperpolarization and smooth muscle relaxation via phosphodiesterase-3 inhibition. Because ACh is never released in significant quantities into the blood in the absence of administered cholinergic agents, the vascular cholinergic receptors have no known function.
Most organs' smooth muscle is contracted (mainly through M3 receptors). Tone and peristalsis in the gastrointestinal tract are increased, while sphincters relax, resulting in abdominal cramps and bowel evacuation.The ureter's peristalsis is increased. The detrusor muscle contracts while the bladder trigone and sphincter relax, resulting in bladder voiding (urination). Bronchial muscles constrict, and asthmatics are hypersensitive, resulting in bronchospasm, dyspnea, and the precipitation of a bronchial asthma attack.
Secretion from all parasympathetically innervated glands including sweating, salivation, lacrimation, and increased tracheobronchial and gastric secretion are all increased via M3 and some M2 receptors. The effect on pancreatic and intestinal glands is minimal. The secretion of milk and bile is unaffected.
ACh is involved in the stimulation of ciliary muscle contraction for near vision as well as the constriction of the pupillae sphincter muscle, which causes miosis (marked constriction of the pupil). During ophthalmic surgery, ACh (1 percent solution) is instilled into the anterior chamber of the eye to cause miosis.
Bethanechol is a carbamoyl ester that is structurally similar to ACh. It is not hydrolyzed by AChE due to carbamic acid esterification, but it is inactivated by other esterases through hydrolysis. Because of the addition of the methyl group, it lacks nicotinic activity but has strong muscarinic activity. It primarily affects are on the smooth musculature of the bladder and GI tract. It has an action time of about an hour.
It has been used to promote urination in postoperative/postpartum nonobstructive urinary retention, neurogenic bladder. Although it can provide symptomatic relief in congenital megacolon and gastroesophageal reflux, it is rarely used for these conditions. The following side effects are common: belching, colic, involuntary urination/defecation, flushing, sweating, drop in blood pressure, and bronchospasm.
Dose: 10–40 mg oral, 2.5–5 mg s.c.;
UROTONIN, BETHACOL 25 mg tab.
Carbachol has muscarinic and nicotinic properties. Carbachol, like bethanechol, is an ester of carbamic acid and a poor substrate for AChE. Other esterases biotransform it, but at a much slower rate.
Because of its ganglion-stimulating activity, carbachol has profound effects on both the cardiovascular and GI systems, and it may first stimulate and then depress these systems. Its nicotinic action can cause the release of epinephrine from the adrenal medulla. It mimics the effects of ACh when injected locally into the eye, causing miosis and a spasm of accommodation in which the ciliary muscle of the eye remains in a constant state of contraction. Carbachol is rarely used therapeutically due to its high potency, receptor nonselectivity, and relatively long duration of action, except in the eye as a miotic agent to treat glaucoma by resulting in pupillary contraction and a drop in intraocular pressure.
The alkaloid pilocarpine is a tertiary amine that is resistant to AChE hydrolysis. It is significantly less potent than ACh and its derivatives, but it is uncharged and can enter the CNS at therapeutic doses. Pilocarpine is a muscarinic agent that is primarily used in ophthalmology.
Pilocarpine is only used in the eye as 0.5–4% drops. It is a third-line treatment for open angle glaucoma. A stinging sensation in the eye, followed by a painful spasm of accommodation, is a common side effect.
It is occasionally used to diagnose bronchial hypersensitivity by acting on muscarinic receptors. Patients who do not have clinically visible asthma are more sensitive to methacholine-induced bronchoconstriction than healthy patients.
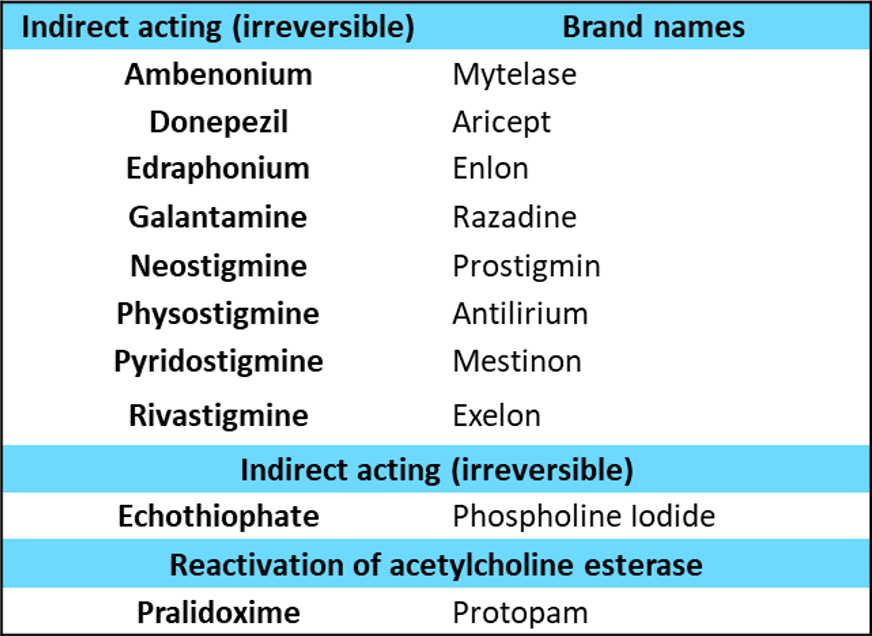
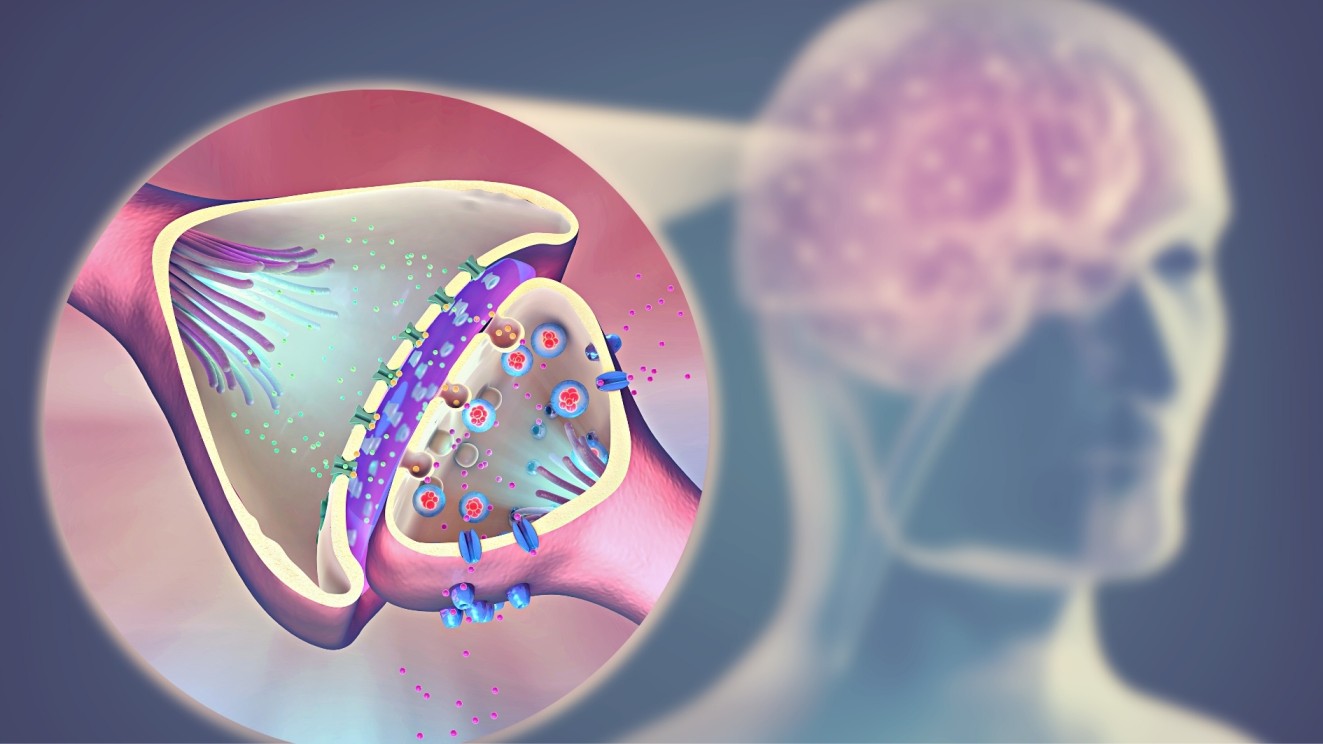
AChE is an enzyme that cleaves ACh to acetate and choline, thereby terminating its actions. It is membrane bound and found both pre- and postsynaptically in the nerve terminal. AChE inhibitors indirectly provide cholinergic action by preventing ACh degradation. As a result, ACh accumulates in the synaptic space. As a consequence, these drugs can elicit a response at all cholinoceptors in the body, including the ANS's muscarinic and nicotinic receptors, as well as the NMJ and the brain. There are two types of indirect acting cholinergic agonists: reversible cholinergic agonists and irreversible cholinergic agonists.
Reversible AChE inhibitors are classified as either short-acting or intermediate-acting agents. The following are the most commonly used reversible drugs:
is a short-acting AChE inhibitor prototype. Edrophonium binds to the active center of AChE in a reversible manner, preventing ACh hydrolysis. Due to rapid renal elimination, it is rapidly absorbed and has a short duration of action of 10 to 20 minutes. Edrophonium is a quaternary amine with a limited range of action to the periphery. It is used to diagnose myasthenia gravis, an autoimmune disease caused by antibodies to the NMJ's nicotinic receptor. As a result, they degrade, leaving fewer receptors available for interaction with ACh. Edrophonium intravenous injection causes a rapid increase in muscle strength. (Atropine), the antidote, must be used with caution because too much of the drug can cause a cholinergic crisis.
Physostigmine is a tertiary amine that is found naturally in plants as a nitrogenous carbamic acid ester. It is an AChE substrate, and it forms a relatively stable carbamoylated intermediate with the enzyme, which is then inactivated reversibly. As a result, cholinergic activity is increased throughout the body.
As a result of its action, physostigmine has a wide range of effects and stimulates not only the muscarinic and nicotinic sites of the ANS, but also the nicotinic receptors of the NMJ. It has an action time of 30 minutes to 2 hours and is classified as an intermediate-acting agent. Physostigmine can enter the CNS and stimulate cholinergic sites.
It is quickly absorbed from the GI tract and parenteral sites. The drug stimulates intestinal and bladder motility, which serves as a therapeutic action in either organ atony. When applied to the eye, it freely penetrates the cornea. It crosses the blood-brain barrier and is excreted after being hydrolyzed by ChE. Ophthalmology departments usually prepare eye drops freshly. BI-MIOTIC 0.25% eye drops with 2% pilocarpine nitrate.
Physostigmine is also used to treat anticholinergic drug overdoses such as atropine.
Neostigmine is a synthetic compound that is also a carbamic acid ester, and it inhibits AChE in a reversible manner similar to physostigmine. In contrast to physostigmine, neostigmine contains quaternary nitrogen. As a result, it is more polar, is poorly absorbed from the GI tract, and does not enter the CNS. It has a stronger effect on skeletal muscle than physostigmine and can stimulate contractility before paralyzing it. Neostigmine has a medium duration of action, lasting between 30 minutes and 2 hours.
It is used to stimulate the bladder and gastrointestinal tract, as well as as an antidote to competitive neuromuscular-blocking agents. Neostigmine is also used to treat myasthenia gravis symptoms.
Pyridostigmine and ambenonium are two other cholinesterase inhibitors used in the long-term treatment of myasthenia gravis. Their action times are intermediate (3 to 6 hours and 4 to 8 hours, respectively) but longer than neostigmine's. Pyridostigmine is similar to neostigmine in every way except that it is less potent and lasts longer, requiring less frequent dosing in myasthenia gravis.
Alzheimer's patients have a cholinergic neuron deficiency in the CNS. This observation prompted the development of anticholinesterases as potential treatments for cognitive function loss. Tacrine was the first to become available, but due to its hepatotoxicity, it has been replaced by others. Despite the ability of donepezil, rivastigmine, and galantamine to postpone the progression of Alzheimer's disease, none of them can stop it. Their main side effect is gastrointestinal distress.
Several synthetic organophosphate compounds have the ability to bind covalently to AChE. As a result, there is a long-term increase in ACh at all sites where it is released. Many of these drugs are extremely toxic and were developed as nerve agents by the military. Insecticides use related compounds such as parathion and malathion.
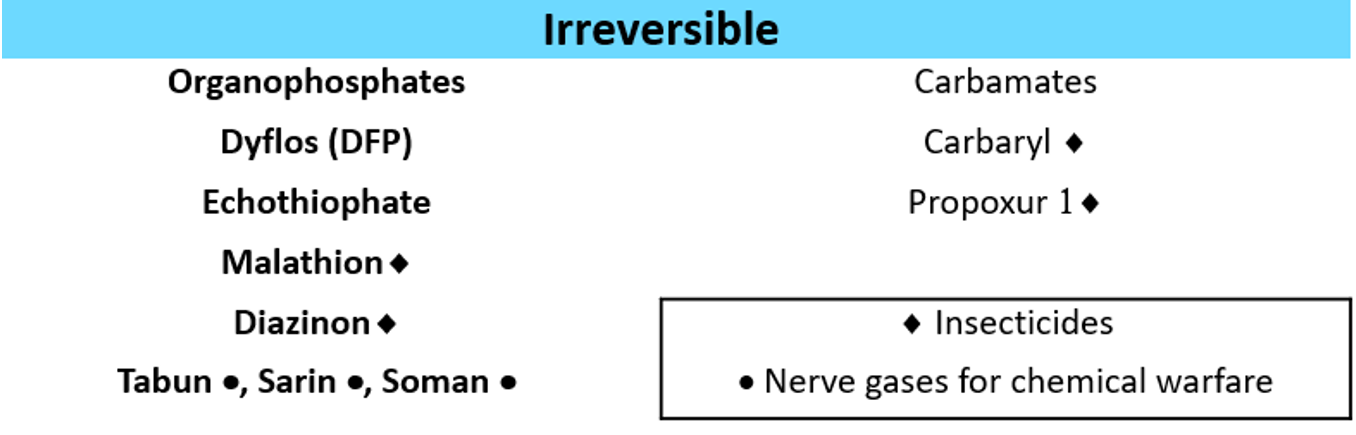
is an organophosphate that covalently binds to the active site of AChE via its phosphate group. When this happens, the enzyme is permanently inactivated, and reactivating it requires the synthesis of new enzyme molecules. The phosphorylated AChE slowly releases one of its ethyl groups after covalent modification. Aging causes chemical reactivators, such as pralidoxime, being unable to break the bond between the remaining drug and the enzyme. Pralidoxime can only reactivate the enzyme for the first 30 minutes. It takes days to hydrolyze the covalent alkylphosphoryl-serine bond.
Echothiophate causes severe miosis and has thus found therapeutic use. For the treatment of open-angle glaucoma, the drug is available as a topical ophthalmic solution. Echothiophate, on the other hand, is rarely used due to its adverse effect profile, which includes the risk of causing cataracts.
1. Whalen, K., Finkel, R. and Panavelil, T.A. (2015). Pharmacology. Philadelphia: Wolters Kluwer.
2. Tripathi, K.D. (2015). Essentials of medical pharmacology. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd.
3. Katzung, B.G. (2018). Basic & clinical pharmacology. 14th ed. New York I 11 Pozostałych: Mcgraw-Hill Education, Copyright.
4. Rosenfeld, G.C. and Loose, D.S. (2014). Pharmacology. Baltimore, Md: Lippincott Williams & Wilkins.
5. Trevor, A.J., Katzung, B.G. and Marieke Kruidering-Hall (2015). Pharmacology examination & board review. New York: Mcgraw-Hill.
Cholinergic drugs act on receptors activated by acetylcholine (ACh), Drugs that affect the autonomic nervous system (ANS) are classified into two groups based on�
The term "cholinergic antagonist" refers to agents that bind to cholinergic receptors (muscarinic or nicotinic) and block the effects of acetylcholine
The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)
Choose what we can use. Strictly necessary and security cookies are always on.