1. What are the Cholinergic Antagonists agents?
2. What are the Antimuscarinic agents?
3. What are the most common Antimuscarinic drugs?
The term "cholinergic antagonist" refers to agents that bind to cholinoceptors (muscarinic or nicotinic) and block the effects of acetylcholine (ACh) and other cholinergic agonists. Cholinoceptor antagonists, like agonists, are classified into muscarinic and nicotinic subgroups based on their receptor affinities. These medications are known as pharmacologic antagonists or inverse agonists. The selective muscarinic receptor blockers are the most clinically useful of these agents. They are also known as anticholinergics, antimuscarinics or parasympatholytics.
Ganglionic blockers, a second class of drugs, prefer the nicotinic receptors of the sympathetic and parasympathetic ganglia. They are the least important cholinergic antagonists in clinical practice.
The neuromuscular-blocking agents (mostly nicotinic antagonists) are a third class of compounds that interfere with the transmission of efferent impulses to skeletal muscles. These agents are used in anesthesia as skeletal muscle relaxant adjuvants during surgery, intubation and various orthopedic procedures.
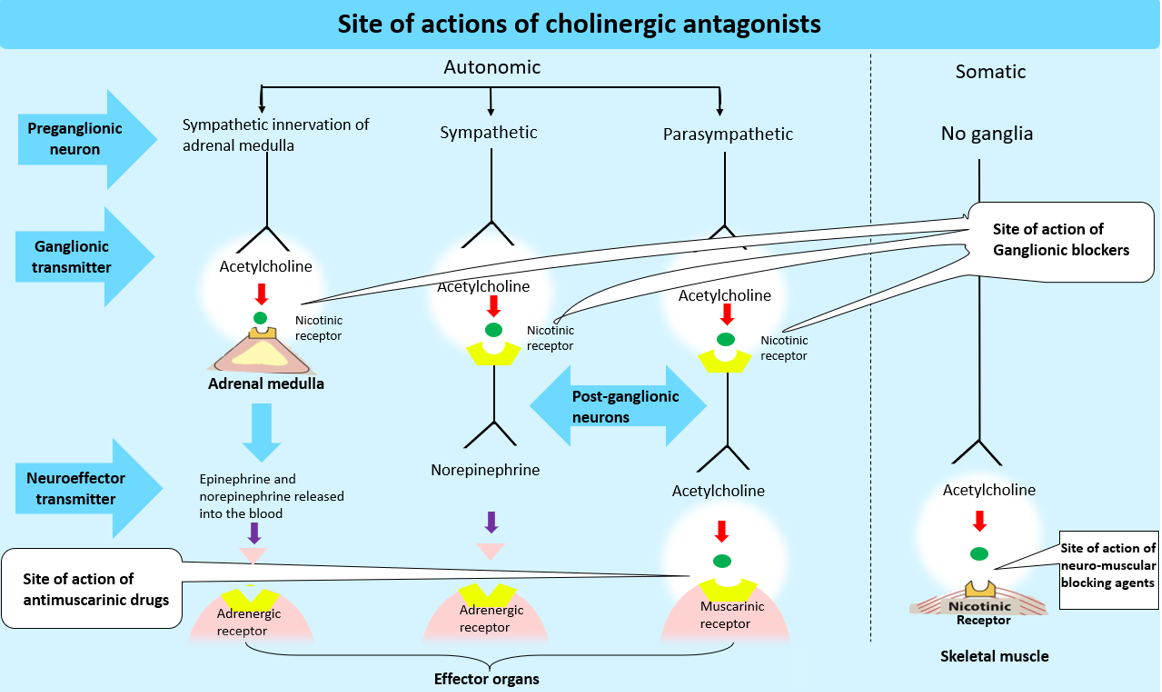
Muscarinic-receptor antagonists, also known as anticholinergic drugs, are competitive antagonists of ACh at all muscarinic cholinoceptors. These agents inhibit muscarinic functions by blocking muscarinic receptors. Furthermore, these medications inhibit the few cholinergic sympathetic neurons that innervate the salivary and sweat glands. Anticholinergic drugs (more precisely, antimuscarinic drugs) have little or no effect on skeletal neuromuscular junctions (NMJs) or autonomic ganglia because they do not block nicotinic receptors.
Muscarinic receptor antagonists are either tertiary amine alkaloids (such as atropine, scopolamine and tropicamide) or quaternary amines (e.g., propantheline [Pro-Banthine], ipratropium [Atrovent]). Tertiary amines are frequently used for their CNS effects. Quaternary amines which have little effect on the CNS, are frequently used for their effects on peripheral systems.
Anticholinergic medications are useful in a variety of clinical situations.
Atropine is the prototype nonselective muscarinic blocker. Atropine is a belladonna alkaloid tertiary amine with a high affinity for muscarinic receptors. It binds competitively to those sites, preventing ACh from binding to them. Atropine has both central and peripheral effects. Atropine, as a tertiary amine, is relatively lipid-soluble and easily crosses membrane barriers. The drug is well distributed throughout the body, including the CNS, the eye, and other organs. It is eliminated partially by metabolism in the liver and partially unchanged in the urine, the half-life is approximately 2 h; and the duration of action of normal doses is 4–8 h, except in the eye, where it may last for days. Atropine sensitivity varies between neuroeffector organs. The greatest inhibitory effects are on bronchial tissue and sweat and saliva secretion.
The actions of atropine can be predicted largely based on knowledge of parasympathetic responses. The effects are most noticeable in organs that normally receive a lot of parasympathetic tone. Atropine inhibits all muscarinic receptor subtypes
Depending on the dose, atropine has varying effects on the cardiovascular system. The main effect at low doses is a slight decrease in heart rate (bradycardia). This effect is caused by the blockade of M1 receptors on inhibitory prejunctional (or presynaptic) neurons, which allows for increased ACh release. By blocking the M2 receptors on the sinoatrial node, higher doses of atropine cause a progressive increase in heart rate.
Atropine has no consistent or significant effect on blood pressure because cholinergic impulses are not involved in the maintenance of vascular tone. Tachycardia and vasomotor center stimulation raise blood pressure, whereas histamine release and direct vasodilator action (at high doses) lower blood pressure. Atropine inhibits the vasodepressant action of cholinergic agonists.
In the past, atropine, methscopolamine and propantheline were used to reduce acid secretion in acid-peptic disease. Although gastric motility is reduced, hydrochloric acid production is unaffected. As a result, atropine is ineffective in the treatment of peptic ulcers. They are also no longer used for this indication because they are ineffective compared to H2 blockers and proton pump inhibitors, and they cause far more frequent and severe side effects.
[It should be noted that pirenzepine, an M1 muscarinic antagonist, does reduce gastric acid secretion at doses that do not interfere with other systems]. Atropine doses that reduce spasms also decrease saliva secretion, ocular accommodation, and urination. These side effects reduce compliance with atropine. Muscarinic blockers can be used to relieve cramping and hypermotility in transient diarrheas but diphenoxylate and loperamide are more effective.
Atropine inhibits muscarinic activity in the eye. Topical atropine instillation causes mydriasis (dilation of the pupil), aversion to light and cycloplegia that lasts 7–10 days. This causes photophobia and (inability to focus for near vision). The ciliary muscles recover slightly faster than the sphincter pupillae. Intraocular tension tends to rise in patients with angle-closure glaucoma. Conventional systemic doses of atropine, on the other hand, have minor ocular effects.
Atropine significantly reduces sweat, salivary, tracheobronchial and lacrimal secretion (M3 blockade). The skin and eyes become dry and speaking and swallowing may become difficult.
Atropine inhibits muscarinic receptors in the salivary glands, causing mouth dryness (xerostomia). Atropine has a high sensitivity in the salivary glands. Sweat and lacrimal glands are both affected in the same way. [Note: Sweat gland secretion inhibition can result in elevated body temperature, which can be dangerous in children and the elderly].
The medication is used to treat bradycardia of various causes. As in the use of these drugs to treat acute myocardial infarction with accompanying bradycardia, hypotension, or arrhythmias.
Atropine is used to relax the GI tract as an antispasmodic agent. Atropine and scopolamine are two of the most powerful antispasmodic medications available.
Topical atropine has both mydriatic and cycloplegic effects, and it allows for the measurement of refractive errors without interference from the eye's accommodative capacity. Antimuscarinics with a shorter duration of action (e.g., homatropine, cyclopentolate [Cyclogyl], tropicamide) that cause mydriasis are administered topically as eye drops or ointments for refractive measurements and ophthalmoscopic examination of the retina and other eye structures, have largely replaced atropine due to the prolonged mydriasis observed with atropine (7 to 14 days vs. 6 to 24 hours with other agents). [Note: If cycloplegia is not required, phenylephrine or similar adrenergic drugs are preferred for pupillary dilation.]
Atropine is sometimes used as an antisecretory agent prior to surgery to block secretions in the upper and lower respiratory tracts.
Atropine is used to treat organophosphate (insecticides, nerve gases) poisoning, anticholinesterase overdoses such as physostigmine, and some types of mushroom poisoning (certain mushrooms contain cholinergic substances that block cholinesterases). To counteract the poisons, massive doses of atropine may be required over a long period of time. The ability of atropine to enter the central nervous system (CNS) is particularly important in the treatment of anticholinesterase central toxic effects.
Side effects are quite common with the use of atropine and its congeners; they are caused by aspects of its action that are not related to the purpose for which it is being used. They are inconvenient but rarely dangerous.
Atropine can cause dry mouth, blurred vision, "sandy eyes", tachycardia, urinary retention and constipation depending on the dose. Restlessness, confusion, hallucinations and delirium are some of the effects on the CNS, which can lead to depression, collapse of the circulatory and respiratory systems, and death. To overcome atropine toxicity, low doses of cholinesterase inhibitors such as physostigmine may be used. Atropine may also cause unpleasant urinary retention. Children may be at risk from the drug because they are more sensitive to its effects, particularly the rapid increases in body temperature that it may cause.
Glaucoma, particularly angle-closure glaucoma, GI and urinary tract obstruction (e.g., prostatic hypertrophy), and gastric ulcer are relative contraindications. Muscarinic-receptor antagonists can produce additive effects when combined with other drugs that have muscarinic-receptor antagonist activity (certain antidepressants, antipsychotics, and antihistamines).

Check out What are the most common Antimuscarinic drugs? article to know the other Antimuscarinic drugs ‼️
1. Whalen, K., Finkel, R. and Panavelil, T.A. (2015). Pharmacology. Philadelphia: Wolters Kluwer.
2. Tripathi, K.D. (2015). Essentials of medical pharmacology. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd.
3. Katzung, B.G. (2018). Basic & clinical pharmacology. 14th ed. New York I 11 Pozostałych: Mcgraw-Hill Education, Copyright.
4. Rosenfeld, G.C. and Loose, D.S. (2014). Pharmacology. Baltimore, Md: Lippincott Williams & Wilkins.
5. Trevor, A.J., Katzung, B.G. and Marieke Kruidering-Hall (2015). Pharmacology examination & board review. New York: Mcgraw-Hill.
Cholinergic agonists act similarly to Acetylcholine, either by directly interacting with cholinergic receptors or by increasing ACh availability at these sites.

In order to understand Antimuscarinic drugs properly, it's required to classify them according to their chemistry.
The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)
Choose what we can use. Strictly necessary and security cookies are always on.