Tubular reabsorption is the mechanism by which water and other substances are transferred back to the blood from the renal tubules. As the glomerular filtrate flows through the nephron tubular portion, both quantitative and qualitative changes occur. Significant volumes of water (more than 99 %), electrolytes, and other substances are reabsorbed by the tubular epithelial cells. Reabsorbed substances pass through the renal medulla interstitial fluid, and the substances move into the blood in peritubular capillaries from there.
Because the substances are brought back into the blood from the glomerular filtrate, the whole process is called tubular reabsorption. For many substances, the mechanism of glomerular filtration and tubular reabsorption is (quantitatively large compared to urinary excretion). This means that a relatively large change in urinary excretion can occur because of a small change in glomerular filtration or tubular reabsorption and, tubular reabsorption is (highly selective), unlike the glomerular filtration, which is relatively nonselective (essentially all solutes in the plasma are filtered except the plasma proteins or substances bound to them).
The urinary excretion rate of some substances is essentially zero, such as (glucose and amino acids), because they are almost entirely reabsorbed from the tubules. Many of the ions in the plasma, such as sodium, chloride, and bicarbonate, are also highly reabsorbed, but their reabsorption and urinary excretion rates differ depending on the body's needs. Waste materials, such as urea and creatinine, are, on the other hand, poorly reabsorbed from the tubules and excreted in relatively large quantities.
For a substance to be reabsorbed, it must first be transferred (1) through the tubular epithelial membrane into the renal interstitial fluid and then (2) through the peritubular capillary membrane back into the blood, the reabsorption of water and solutes includes a series of transport steps.
The basic transport mechanisms involved in tubular reabsorption are two types:
Reabsorption through the tubular epithelium into the interstitial fluid requires active or passive transport. For example, water and solutes can be transported through the cell membranes themselves (transcellular route) or through spaces between the cell junctions (paracellular route).
Then water and solutes are transferred through the peritubular capillary walls into the blood through ultrafiltration (bulk flow), After absorption through the tubular epithelial cells into the interstitial fluid. Mediated through hydrostatic and colloid osmotic forces. The peritubular capillaries function like the venous ends of most other capillaries since there is a net reabsorptive force that transfers fluids and solutes from the interstitium to the blood.
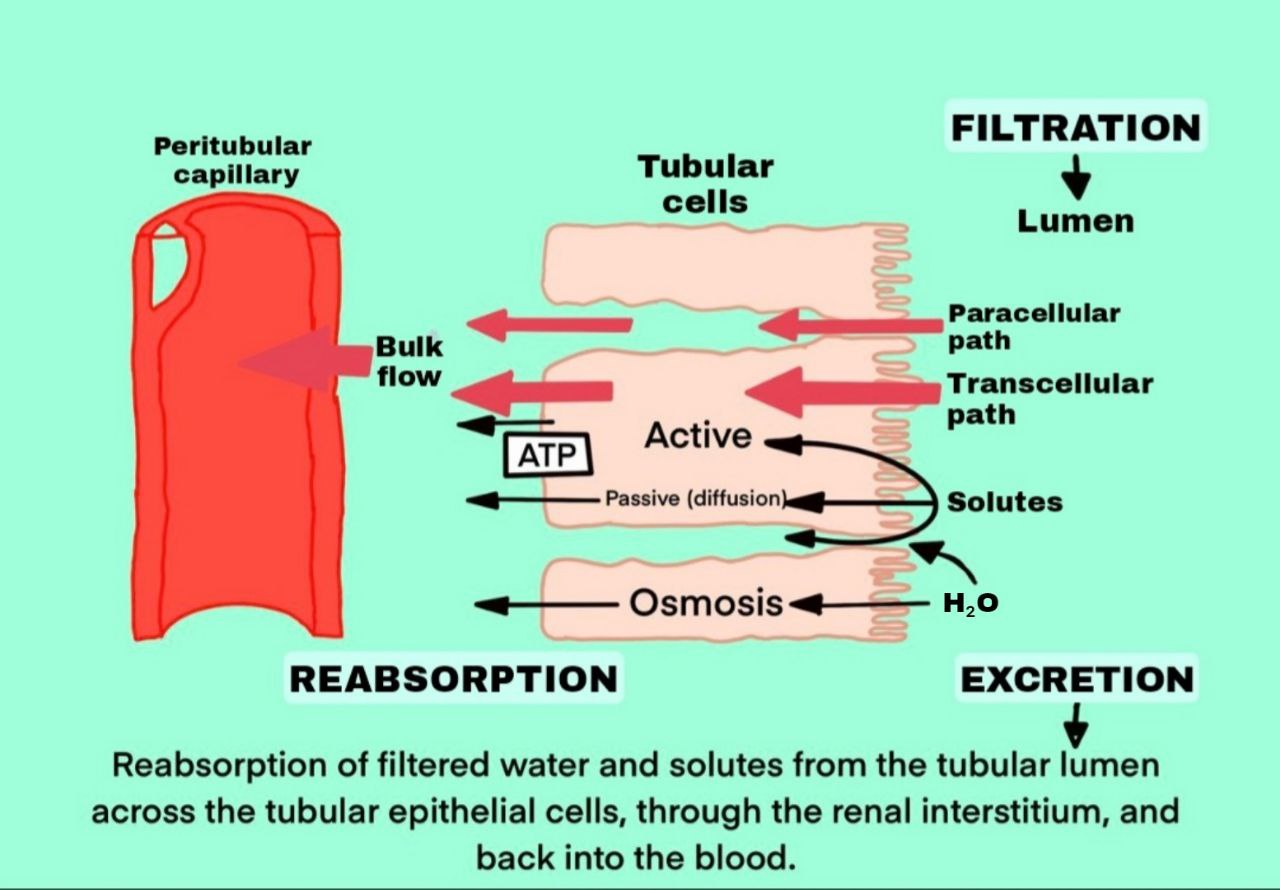
Active transport is the movement of molecules against the electrochemical gradient and involves energy extracted from metabolism. Transport that is directly connected to an energy source, such as adenosine triphosphate hydrolysis (ATP), is referred to as primary active transport. A good example of this is the sodium-potassium ATPase pump, which functions throughout most parts of the renal tubule, other Substances reabsorbed actively from the renal tubule are calcium, phosphate, sulfates, bicarbonate, glucose, amino acids, ascorbic acid, uric acid, and ketone bodies.
Transport that is indirectly connected to an energy source, such as that due to an ion gradient, is referred to as secondary active transport. An example of secondary active transport is the reabsorption of glucose by the renal tubule. Although the solutes can be reabsorbed by tubule in active and/or in passive mechanisms. Water is always reabsorbed by osmosis which is a passive (non-active) physical mechanism.
Solutes can be moved against their electrochemical gradient, because of the special ability of the primary active transport. The energy for this active transport comes from the hydrolysis of ATP via membrane-bound ATPase; ATPase is also a component of the carrier mechanism that binds and moves solutes across cell membranes. Sodium potassium ATPase, hydrogen ATPase, hydrogen potassium ATPase, and calcium ATPase are the primary active transporters in the kidneys that are known.
In secondary active transport, two or more substances interact with a particular membrane protein (a carrier molecule) and are transported together through the membrane. If one of the substances (e.g., sodium) diffuses down its electrochemical gradient, the energy released is used to force another substance (e.g., glucose) against its electrochemical gradient.
Consequently, secondary active transport does not require energy directly from ATP or from other high energy phosphate sources. Rather, the simultaneous facilitated diffusion of another transported substance down its own electrochemical gradient liberates the direct source of the energy.
The movement of molecules along the electrochemical gradient is referred to as Passive reabsorption. This process does not involve energy and occurs spontaneously by the following mechanisms:
Reabsorption of the substances occurs in almost all the segments of the tubular portion of nephron.
Approximately 7/8 of the filtrate (about 88 %) is reabsorbed in the proximal convoluted tubule. The brush border of epithelial cells in proximal convoluted tubules increases the surface area and promotes reabsorption. Reabsorbed substances from proximal convoluted tubules are sodium, potassium, calcium, bicarbonate, chloride, phosphate, urea, uric acid (almost all glucose and amino acids), and water. This segment does not reabsorb inulin, creatinine sucrose, and mannitol.
About 20% of filtered Na+ and Cl−, 15% of filtered water and cations such as K+, Ca2+ and Mg2+ are reabsorbed in the loop of Henle. In different parts of the loop of Henle Reabsorption can occur:
Thin descending limb of the loop of Henle
Exclusively in this part of the loop of Henle, water absorption occurs passively (because of hypertonic interstitial fluid). It is achieved by the diffusion of sodium ions from the interstitial fluid into the tubular lumen.
Thin ascending limb of the loop of Henle
Limited passive reabsorption of Na+ and Cl− occurs in this water-impermeable limb. The fluid leaving this limb is hypotonic relative to plasma, because of impermeability to water.
Thick ascending limb of the loop of Henle
This limb is impermeable to water but is involved in the reabsorption of 25% of the filtered Na+, Cl−, and potassium, as well as large amounts of calcium, bicarbonate, and magnesium. This segment also secretes hydrogen ions into the tubular lumen. About half of the Na+ is reabsorbed actively and transcellularly, while the other half of the Na+ is reabsorbed passively by paracellular pathway along with other cations.
Sodium, calcium, bicarbonate, and water are reabsorbed from the distal convoluted tubule. Approximately 7% of the filtered NaCl and about 8–17% of water is reabsorbed by the Distal Convoluted Tubule, early distal tubule (the initial segment of distal tubule) reabsorbs Na+, Cl−, Ca2+, and is impermeable to water.
1.GUYTON AND HALL, Textbook of Medical Physiology, 12th edition, Jackson Mississippi, University of Mississippi Medical Center, [2011]
2.K SEMBULINGAM AND PREMA SEMBULINGAM, Essentials of Medical Physiology, Sixth Edition, New Delhi, Panama City, London, Dhaka, Kathmandu, JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD, [2012]
3.INDU KHURANA AND ARUSHI KHURANA, Textbook of Medical Physiology, 2nd Edition, India, Elsevier India, [December 1, 2015]
4.JOHN FEEHALLY, JÜRGEN FLOEGE, MARCELLO TONELLI, RICHARD J. JOHNSON, Comprehensive Clinical Nephrology, Sixth Edition, Edinburgh, London, New York, Oxford, Philadelphia, StLouis, Sydney, Elsevier, [September 11, 2018]
5.VALERIE C. SCANLON, TINA SANDERS, Essentials of Anatomy and Physiology, fifth edition, New York, F. A. Davis Company, [January 1, 2006]
6.KIM E. BARRETT, SUSAN M. BARMAN, HEDDWEN L. BROOKS, JASON YUAN, Ganong's Review of Medical Physiology, 26th edition, New York, Chicago, San Francisco, Athens London, Madrid, Mexico City, Milan, New Delhi, Singapore, Sydney, Toronto, Mc Graw Hill Education, [January 29, 2019]
7.ANNE WAUGH, ALLISON GRANT, Ross and Wilson ANATOMY and PHYSIOLOGY in Health and Illness, 11th edition, Edinburgh, London, New York, Oxford, Philadelphia, St Louis Sydney, Toronto, Churchill Livingstone, [September 7, 2010]
Urine formation happens in three major steps, The first step is glomerular filtration, which is followed by the tubular reabsorption and the tubular secretion. Click here to read about these steps in detail.

The Renal tubule is a long, complicated tubule, about 15 mm long and 55 μm in diameter. The tubular portion of the nephron is the continuation of...

The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)