Note: To read part 1, click here.
Nephrons, collecting ducts (CDs) and a unique microvasculature are the basic components of the kidney. A nephron is classified as the structural and functional unit of the kidney. The size of the kidneys varies from one species to another, as does the number of nephrons they contain.
Each human kidney has approximately 1 million nephrons capable of producing urine. This number varies considerably, however. The number of nephrons is already formed during embryonic development; new nephrons cannot develop after birth and the missing nephron cannot be replaced (the kidney cannot regenerate new nephrons). Therefore, with renal injury, disease, or normal aging, there is a gradual decline in the number of nephrons.
After age 40, the number of functioning nephrons typically decreases by around 10% per 10 years; thus, at age 80, many people have 40% less functioning nephrons than at age 40. This loss is not life-threatening, since the adaptive changes in the remaining nephrons allow them to excrete the appropriate quantities of water, electrolytes, and waste products.
It is in the nephrons, with their associated blood vessels, that urine is formed.
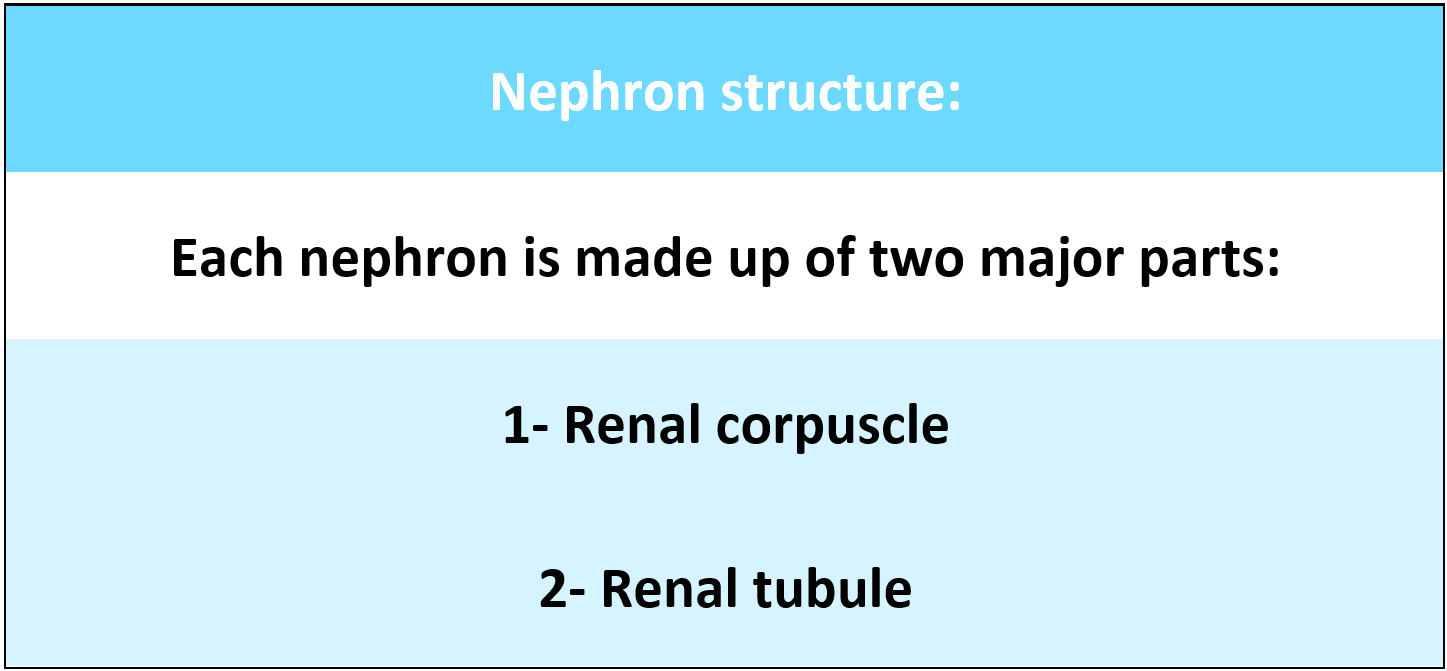
Each nephron has two major portions(parts):
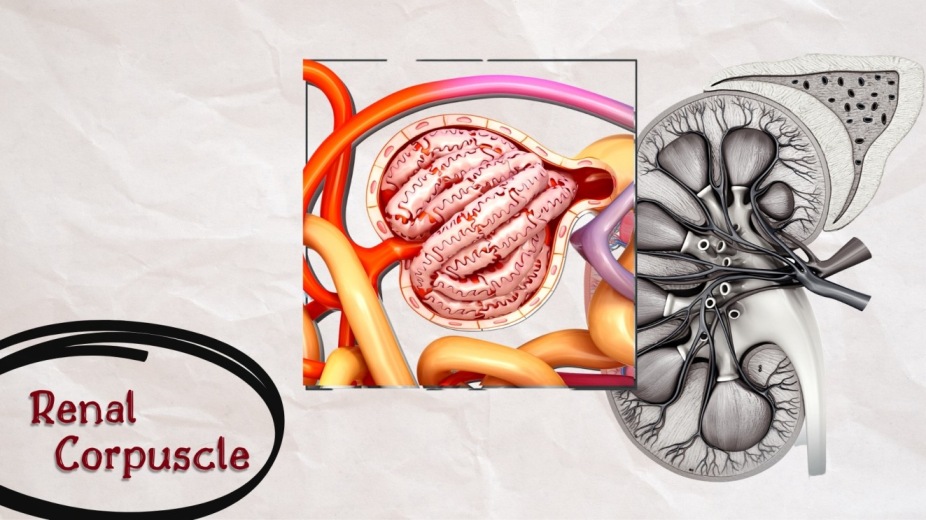
The renal corpuscle is located in the cortex of the kidney, either near the periphery or near the medulla. The function of the renal corpuscle is to filter the blood that forms the first phase of urine formation.
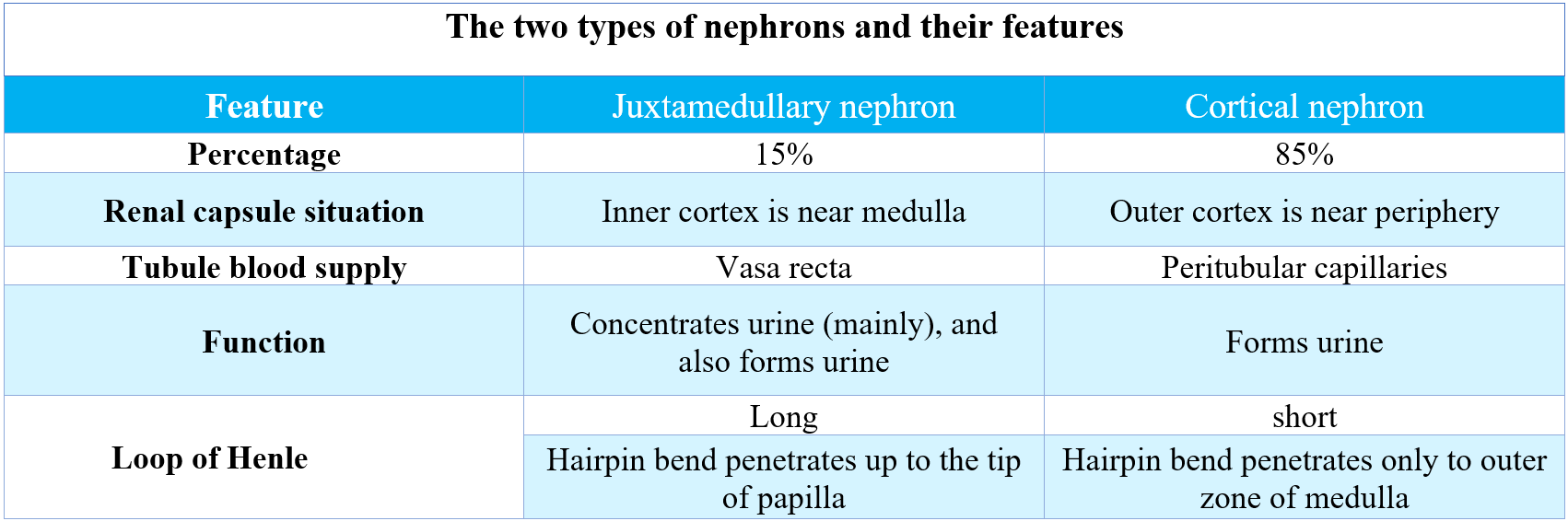
Based on the situation of the renal corpuscle, nephrons are classified into two types:
The renal corpuscle is formed by two portions:
The Renal tubule is a long, complicated tubule, about 15 mm long and 55 μm in diameter. The tubular portion of the nephron is the continuation of the Bowman capsule and consists of the following parts:
Blood vessels of the kidneys are highly specialized to promote the role of nephrons in the production of urine. Similarly, the microvascular structure of the kidney is arranged in mammalian species. Blood flow to the two kidneys is typically around 22 percent of the cardiac output or 1100 ml/min.
The Renal artery arises directly from the abdominal aorta, for the blood to reach the kidneys, it passes from the aorta through the (right and left renal arteries) The renal arteries join the kidney through the hilum. When going through the renal sinus, the renal artery splits into several (segmental arteries). The Segmental artery subdivides into (interlobar arteries) the interlobar artery passes through the medullar pyramids. At the base of the pyramid, it turns and runs parallel to the base of the pyramid (arcuate artery), That runs at right angles to the parent interlobar arteries.
They lie parallel to the kidney surface at the junction of the pyramid and the cortex. Each arcuate artery produces interlobular arteries (cortical radial arteries). Interlobular arteries run through the renal cortex, which is perpendicular to the arcuate artery. No arteries are penetrating the medulla. Numerous (afferent arterioles) arise from each interlobular artery.
Each afferent arteriole enters the Bowman capsule and divides into a rounded tuft of anastomosing capillaries called (glomerulus). Where large amounts of fluids and solutes are filtered to begin the formation of urine, this capillary network has special features that make it work as a sieve allowing plasma filtration with the retention of plasma proteins and blood cells. The distal ends of the capillaries of each glomerulus are joined together to form the (efferent arteriole).
The renal circulation is unique in having two capillary beds, the glomerular and peritubular capillaries, arranged in series and separated by efferent arterioles, which help to regulate the hydrostatic pressure in both capillaries.
The pattern of the renal venous system is similar to that found in the end arterial system, except for the presence of multiple anastomoses between veins at all levels of venous circulation and the lack of a venous system (segmental vain).
Peritubular capillaries and vasa recta empty into the veins of the venous system the corresponding veins which run parallel to the arterial vessels are the interlobular veins, the arcuate veins, the interlobar veins, and the renal veins that exit the kidney at the hilus and join the inferior vena cava.
Each renal tubule and its glomerulus is a unit (nephron), the nephron is the functional unit of the kidney, as described in part one of the renal system physiology. Each human kidney contains about 800,000 to 1,000,000 nephrons, but this number can vary significantly due to renal damage, illness, and aging, the kidneys lack the ability of reproducing new nephrons. The two main portions of each nephron are the Renal corpuscle and the renal tubule. The renal corpuscle is where blood filtration starts. There are two types of nephrons depending on the location of the renal corpuscle the Cortical nephrons and the Juxtamedullary nephrons.
The renal tubule itself can be divided into the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct. Each nephron has a unique region called the juxtaglomerular apparatus which is involved in regulating blood pressure and the rate of glomerular filtration. Located very near to the glomerulus, and has three types of cells Macula densa cells, Juxtaglomerular cells, and extraglomerular mesangial cells.
The pathway of blood flow through the kidney is an essential part of the process of urine formation. Blood from the abdominal aorta enters the renal artery which branches extensively into smaller arteries that give rise to afferent arterioles in the renal cortex. From the afferent arterioles, blood flows into the glomeruli (capillaries), to efferent arterioles, to peritubular capillaries, to veins within the kidney, to the renal vein, and finally to the inferior vena cava.
Notice that in this pathway there are two sets of capillaries, and recall that it is in capillaries that exchanges take place between the blood and surrounding tissues. All these unique physiological anatomies of the nephrons are the reason behind that each nephron capable of forming urine. Now that every detail about the nephrons is known, knowing how urine is formed can be easier, read part 3 of the renal system physiology to know how urine is formed.
1. GUYTON AND HALL, Textbook of Medical Physiology, 12th edition, Jackson, Mississippi, University of Mississippi Medical Center, [2011]
2. K SEMBULINGAM AND PREMA SEMBULINGAM, Essentials of Medical Physiology, Sixth Edition, New Delhi, Panama City, London, Dhaka, Kathmandu, JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD, [2012]
3. INDU KHURANA AND ARUSHI KHURANA, Textbook of Medical Physiology, 2nd Edition, India, Elsevier India, [December 1, 2015]
4. JOHN FEEHALLY, JÜRGEN FLOEGE, MARCELLO TONELLI, RICHARD J. JOHNSON, Comprehensive Clinical Nephrology, Sixth Edition, Edinburgh, London, New York, Oxford, Philadelphia, StLouis, Sydney, Elsevier, [September 11, 2018]
5. VALERIE C. SCANLON, TINA SANDERS, Essentials of Anatomy and Physiology, fifth edition, New York, F. A. Davis Company, [January 1, 2006]
6. KIM E. BARRETT, SUSAN M. BARMAN, HEDDWEN L. BROOKS, JASON YUAN, Ganong's Review of Medical Physiology, 26th edition, New York, Chicago, San Francisco, Athens, London, Madrid, Mexico City, Milan, New Delhi, Singapore, Sydney, Toronto, Mc Graw Hill Education, [January 29, 2019]
7. ANNE WAUGH, ALLISON GRANT, Ross and Wilson ANATOMY and PHYSIOLOGY in Health and Illness, 11th edition, Edinburgh, London, New York, Oxford, Philadelphia, St Louis Sydney, Toronto, Churchill Livingstone, [September 7, 2010]
While various organs are involved in the removal of waste from the body, their excretory capacity is limited. Nevertheless, the renal or urinary system has the highest excretory capacity

The renal corpuscle is formed by two parts: 1. Glomerulus 2. Bowman capsule (glomerular capsule), Glomerulus is a tuft of capillaries enclosed by bowman capsule.
The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)