The kidneys produce urine in order to excrete waste products and to control the volume, electrolytes, and pH of blood and tissue fluid. Urine formation starts with the creation of a plasma ultrafiltrate.
The kidneys, along with water, excrete unnecessary substances from the blood as urine. Urine is clear and amber in color due to the presence of urobilin, a bile pigment altered in the intestine, reabsorbed and excreted by the kidneys. Normal urinary production is 1 L / day to 1.5 L / day.
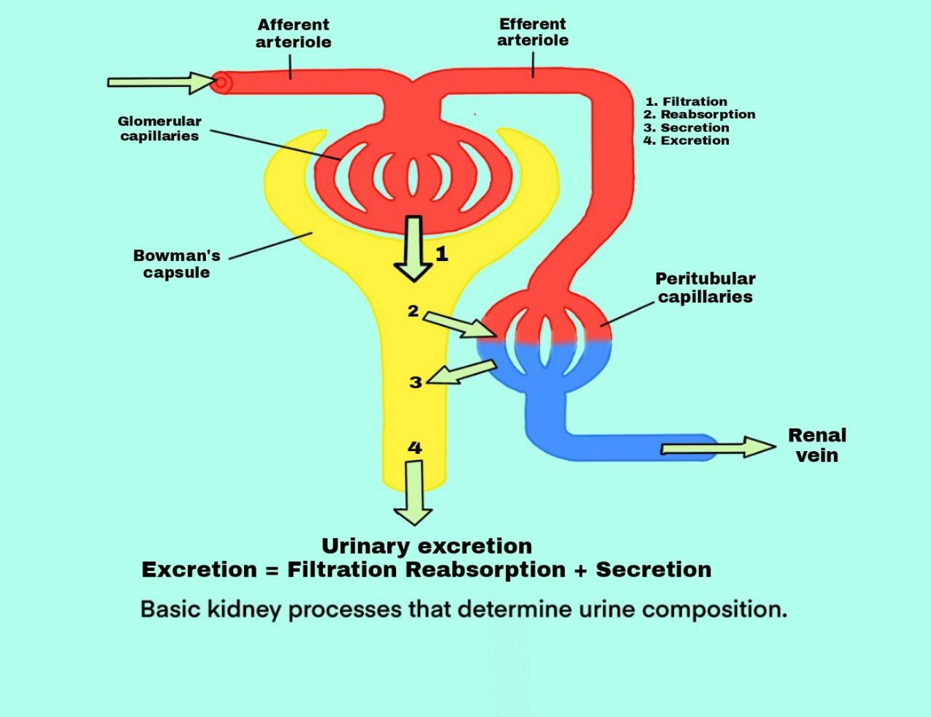
Urine formation happens in three major steps, The first is glomerular filtration, which happens in the renal corpuscles. The second and third are the reabsorption and the secretion of the tubules in the renal tubules.

The rate at which various substances are excreted in the urine is the sum of three renal processes (1) glomerular filtration, (2) reabsorption of substances from the renal tubules into the blood and (3) secretion of substances from the blood into the renal tubules.
Urine formation occurs when a significant volume of fluid that is practically protein-free is filtered from the glomerular capillaries to the Bowman capsule. Most plasma compounds, except proteins, are freely filtered such that their concentration in the glomerular filtrate in the Bowman capsule is approximately the same as in the plasma. As the filtered fluid exits the Bowman capsule and moves into the tubules, it is modified by the reabsorption of many desired substances such as glucose, amino acids, water, and electrolytes from the tubules back into the blood, or by the secretion of certain undesirable substances into the tubule from the peritubular capillaries.
The kidneys produce the urine that passes through the ureters to the bladder for storage before excretion. Urine composition represents the exchange of substances between the nephron and the blood in the renal capillaries. Waste products of protein metabolism are excreted, electrolyte levels are regulated, and pH (acid-base balance) is preserved by the excretion of hydrogen ions.
Glomerular filtration is the first step in the formation of urine. It occurs through a membrane filtration structure is well suited for filtration.
Glomerular filtration refers to the process of ultrafiltration of plasma from the glomerular capillaries to the Bowman capsule. Filtration is a process in which blood pressure pushes plasma and dissolved material out of the capillaries. In glomerular filtration, blood pressure pushes plasma, dissolved substances and small proteins out of the glomeruli and into Bowman’s the capsules. The Filtered fluid is called glomerular filtrate.
All plasma substances are filtered except for plasma proteins and cellular components, including red blood cells. The large molecular size prevents the plasma proteins from being filtrated. The protein molecules are larger than the slit pores found in the capillary endothelium. The Concentrations of other glomerular filtrate components, like certain salts and organic molecules, are similar to plasma concentrations.
Exceptions to this generalization include a few low molecular-weight compounds, such as calcium and fatty acids, which are not straightforwardly filtered since they are partially bound to plasma proteins. For example, almost half of the plasma calcium and most of the plasma fatty acids are bound to proteins and these bound parts are not filtered through the glomerular capillaries.
The glomerular capillary membrane is similar to that of other capillaries, except that it has three (instead of the usual two) major layers: (1) the endothelium of the capillary, (2) the glomerular basement membrane (GBM), and (3) the Bowman visceral epithelium (podocytes) surrounding the outer surface of the capillary basement membrane. Together, these layers make up the filtration barrier, which, despite the three layers, remove several hundred times as much water and solutes as the normal capillary membrane. Even with this high filtration rate, the glomerular capillary membrane normally prevents the filtration of plasma proteins.
The high filtration rate across the glomerular capillary membrane is partly due to its special characteristics. Similar to the fenestrated capillaries found in the liver, the capillary endothelium is perforated by thousands of small holes called fenestrae, endothelial cells are richly endowed with fixed negative charges that hinder the passage of plasma proteins. Although the fenestrations are relatively large.
The endothelium is surrounded by a basement membrane, consisting of a meshwork of collagen and proteoglycan fibrillae, which have large spaces into which large quantities of water and small solutes can filter. The basement membrane effectively prevents the filtration of plasma proteins, partially due to high negative electrical charges associated with proteoglycans.
Is a layer of epithelial cells that line the outer surface of the glomerulus. It is the final portion of the glomerular membrane. the outer surface of the capillaries has a long foot-like process called (podocytes) encircling it, and they are not continuous cells, the foot process is divided by gaps called slit pores through which the glomerular filtrate passes. The epithelial cells, which are also negatively charged, have additional constraints on the filtration of plasma proteins. Thus, plasma proteins filtration is provided by a barrier from all the layers of the glomerular capillary wall.
Owing to its porous existence, the glomerular membrane is extremely permeable to water and 100% to dissolved substances.
The filtration membrane has a high degree of permeability selectivity based on two factors:
1. Pore size: The capillary endothelial cells have pores that are 70–90 nm in diameter, the glomerular basement membrane (GBM) has no pores, however their permeability is 8 nm in pore size and the podocytes form filtration slits that are approximately 25 nm in width. It is evident from this that the glomerular filtration barrier for solutes is at the GBM level. The permeability of the membrane to different neutral solutes, depending on their effective molecular diameter, is as follows:
2. Electrical charge: The permeability of the filtration membrane is not simply related to molecular size, but also to its shape and electrical charge. due to the presence of glycoproteins rich in sialic acid, the pores in the filtration membrane are negatively charged. Thus, with the same molecular size relative to anionic particles, the permeability of neutral and cationic particles is improved. This shows why albumin (with a molecular diameter of 7 nm but with a negative charge) is not filtered.
The glomerular filtration rate (GFR) is defined as the total amount of filtrate produced in all nephrons of both kidneys in the given unit of time. The normal GFR is 125 mL/minute or approximately 180 L/day.
Read about GFR in detail
Of the 180 L glomerular filtrate produced per day, approximately 1.5 L (i.e., < 1 %) is excreted as urine per day. The various segments of the renal tubule. The proximal tubule, the loop of Henle, the distal tubule, and the collecting duct determine the composition and volume of the urine by selective reabsorption of solutes and water and selective secretion of solutes.
As a result, the volume, osmolality, composition, and pH of the intracellular and extracellular fluid compartments are precisely regulated by the tubules. in the determination of the final urinary excretion rate, the tubular reabsorption plays a much more important role for many substances than secretion. However, significant amounts of potassium ions, hydrogen ions, and a few other substances that appear in the urine are secreted by the means of Tubular secretion.
Tubular reabsorption is the mechanism by which water and other substances are transferred back to the blood from the renal tubules. As the glomerular filtrate flows through the nephron tubular portion, both quantitative and qualitative changes occur.
Basic transport mechanisms which are involved in tubular reabsorption are of two types:
Reabsorption of the substances occurs in almost all the segments of the tubular portion of nephron. Those tubular portions include Proximal Convoluted Tubule, Loop of Henle and Distal Convoluted Tubule.
Read about tubular reabsorption in detail.
In tubular secretion, substances are actively secreted from the blood in the peritubular capillaries to the filtrate in the renal tubules, also called tubular excretion. This is the addition of a material to the glomerular filtrate. In addition to the reabsorption of renal tubules, certain compounds are also excreted from the peritubular capillaries into the lumen through the tubular epithelial cells. the first substance was Dye phenol red found to be secreted in renal tubules in experimental conditions. Many other substances later were found to be secreted, such as:
The active secretion of substances occurs in the tubular fluid with the help of certain nonselective carriers. The carrier which secretes para- amino hippuric (PAH) acid can also secrete uric acid, bile acids, oxalic acid, penicillin, probenecid, cephalothin, and furosemide. It is because of the common carrier that probenecid can block the secretion of penicillin and maintain its plasma concentration for a longer time. For bases, there is another carrier, which is also non-selectively involved in the secretion of substances like acetylcholine, creatinine, dopamine, histamine, 5HT, thiamine, quinine, procaine, morphine, and other bases.
Besides to reabsorbing solutes and water, proximal tubule cells also secrete organic anions and cations, which include some end-products of metabolism circulating in plasma, exogenous organic compounds, ammonia, and certain drugs. Potassium is actively secreted by sodiumpotassium pumps in proximal and distal convoluted tubules and by collecting ducts. Hydrogen ions are also excreted by proximal and distal convoluted tubules. Maximum hydrogen ion secretion occurs in the proximal tubule. the loop of Henle secrets urea. Urine is therefore produced in the nephron by glomerular filtration, selective reabsorption, and tubular secretion processes.
Urine formation happens in three steps, glomerular filtration, tubular reabsorption, and tubular secretion.
Glomerular filtration occurs from the glomerulus to Bowman’s capsule. Filtration is primarily determined by the molecular size and shape of the filtered solute and, to a lesser degree by its charge, the blood cells and large proteins remain in the blood. GFR is between 100 and 125 ml per minute. When the glomerular filtrate reaches the renal tubules, it passes sequentially into the successive sections of the tubule, the proximal tubule, the loop of Henle, the distal tubule, the collecting tubule, and, eventually, the collecting duct before it is excreted as urine. Some compounds are selectively reabsorbed back into the blood from the tubules, while others are secreted from the blood to the tubular lumen.
Tubular reabsorption occurs from the filtrate in the renal tubule to the blood in the peritubular capillaries 99 % of the filtrate is reabsorbed only 1% becomes urine. In terms of usefulness, the tubular reabsorption is selective. Nutrients reabsorbed by active transport are glucose, amino acids, and vitamins, and they may have a renal threshold. Positive ions are reabsorbed by (active transport) and negative ions are most commonly reabsorbed by (passive transport). Small proteins are reabsorbed by (pinocytosis), and water is reabsorbed by (osmosis).
Tubular secretion occurs from the blood in the peritubular capillaries to the filtrate in the renal tubule; creatinine and other waste products may be secreted into the filtrate to be excreted in the urine; the secretion of H + ions help to preserve the pH of the blood. With all these changes, the filtrate eventually becomes urine.
1. GUYTON AND HALL, Textbook of Medical Physiology, 12th edition, Jackson, Mississippi, University of Mississippi Medical Center, [2011]
2. K SEMBULINGAM AND PREMA SEMBULINGAM, Essentials of Medical Physiology, Sixth Edition, New Delhi, Panama City, London, Dhaka, Kathmandu, JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD, [2012]
3. INDU KHURANA AND ARUSHI KHURANA, Textbook of Medical Physiology, 2nd Edition, India, Elsevier India, [December 1, 2015]
4. JOHN FEEHALLY, JÜRGEN FLOEGE, MARCELLO TONELLI, RICHARD J. JOHNSON, Comprehensive Clinical Nephrology, Sixth Edition, Edinburgh, London, New York, Oxford, Philadelphia, StLouis, Sydney, Elsevier, [September 11, 2018]
5. VALERIE C. SCANLON, TINA SANDERS, Essentials of Anatomy and Physiology, fifth edition, New York, F. A. Davis Company, [January 1, 2006]
6. KIM E. BARRETT, SUSAN M. BARMAN, HEDDWEN L. BROOKS, JASON YUAN, Ganong's Review of Medical Physiology, 26th edition, New York, Chicago, San Francisco, Athens London, Madrid, Mexico City, Milan, New Delhi, Singapore, Sydney, Toronto, Mc Graw Hill Education, [January 29, 2019]
7. ANNE WAUGH, ALLISON GRANT, Ross and Wilson ANATOMY and PHYSIOLOGY in Health and Illness, 11th edition, Edinburgh, London, New York, Oxford, Philadelphia, St Louis Sydney, Toronto, Churchill Livingstone, [September 7, 2010]
The glomerular filtration rate (GFR) is defined as the total amount of filtrate produced in all nephrons of both kidneys in the given unit of time.

Tubular reabsorption is the mechanism by which water and other substances are transferred back to the blood from the renal tubules. Read about the mechanisms of reabsorption as well as the site at which it happens.
The urethra is a muscular canal that extends from the neck of the bladder to the exterior of body. Read more about the anatomy of urethra in this article.

Dosage guide of Lisinopril: Click to read about the dose for your specific condition and age group.

Learn about medical uses, safety profile, mechanisms and interactions of statins.

Comprehensive guide on Ozempic (semaglutide), including its uses, dosage, side effects, warnings, and interactions.
.png)